Use of Inotropes.
OK, so now we can measure inotropy, can we use it to treat patients appropriately? Well yes, we can. Let’s look at some examples of septic shock in children.
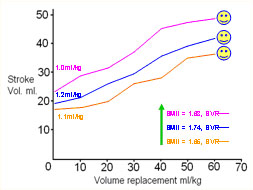
The figure below shows the stroke volume (expressed as ml/kg) and the SMII after 40ml/kg volume resuscitation, for three patients who were typical “fluid responders”.
In contrast, three children failed to show clinical or haemodynamic improvement with volume resuscitation. Their traces are shown below.
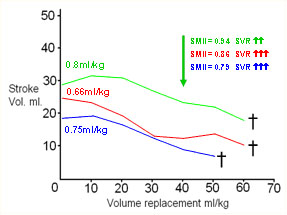
These patients had stroke volumes at presentation below 1ml/kg and had an SMII of less than 1.0W/m2 after 40ml/kg of fluid. Both SV and SMII are therefore showing clear evidence of heart failure. The CI for each patient was 2.3 L/min/m2 (green), 2.1 L/min/m2 (red) and 1.9 L/min/m2 (blue). At 60 ml/kg, the CI values were 1.60 and 1.35 L/min/m2 respectively (child three did not reach 60ml/kg). All had SVRI values greater than 2,800 at 40 ml/kg and for the two who reached it, over 3,600 at 60 ml/kg.
The following figure shows the clinical course of two further patients who initially appeared to be non-responders to fluid alone, and their response to dobutamine at 10 and 15 mcg/kg/min respectively. Both children survived.
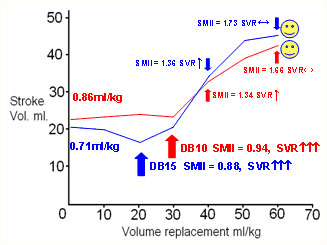
In the first case (red line) there was no significant increase in stroke volume after 30ml/kg. The SMII was 0.94W/m2 and dobutamine was commenced at 10mcg/kg/min. At 40 ml/kg and 60 ml/kg the SMII was 1.34 and 1.66 respectively.
In the second case (blue line) the SMII after 20 ml/kg was 0.88 W/m2 and dobutamine was commenced at 15mcg/kg/min. At 40 and 60 ml/kg the SMII was 1.36 and 1.73 respectively.
The CI values were 2.35 and 2.15 L/min/m2 respectively for each patient prior to the commencement of dobutamine. After 60 ml/kg, with dobutamine still infusing, the figures were 4.4 and 4.7 L/min/m2 respectively.
From the above it would appear that septicaemic shock in these particular children presents with a low stroke volume (and consequently low CI) which may be due to inadequate preload and which responds to volume challenge, or from a combination of low preload and myocardial depression which may not respond to fluid alone. In effect, the non-responders appear to be on a lower, flatter Frank-Starling curve.
If we want to increase stroke volume when there is enough preload but in the face of cardiac failure, then we have to use inotropes. But which one?
As both of the non-responders who received dobutamine had very high SVRI values of 3,300 and 3,450 respectively, a vaso-dilating inotrope seemed a logical choice; hence dobutamine was selected in preference to noradrenaline or dopamine. Other cases may well show a different pattern of SVRI, more like the low vascular resistance/high cardiac output cases often seen in adult septicaemia, where a vasoconstricting inotrope would be a more appropriate choice, but a logical choice of inotrope can always be made on the basis of the CI, SMII and SVRI.
We should ask three questions:
1). Is the CI high, low or normal?
2). Is the SVRI high, low or normal.
3). Is the SMII normal or low?
More simply, do we need to increase inotropy, and do we need vasodilation or vasoconstriction? There is no need for, or justification for, empiric treatment. We can measure the necessary variables. The only problem is can we achieve the result we want with the use of a single agent? Unfortunately, while the answer is often yes, frequently it is no. In these cases we have to use balanced inotropes.
|

