Balancing Inotropes.
Let’s look at an example of severe septicaemia. As you’ve probably gathered by now, septicaemia really is the “happy hunting ground” of haemodynamics!
This 57 year old, 87kg male presented to ED with a BP of 72/44 and a history of collapse at home.
His pulse rate was 136, his temperature 38.8, white cell count was 26,000 and his PaO2 was 64mmHg and his SpO2 94% on approximately 80% inspired oxygen. He was treated in ED by “aggressive fluid resuscitation” in the form of normal saline 4 litres over 80 minutes. His BP rose a little to 76/47, and his pulse rate fell to 106. Here is his initial USCOM result. What do you see?
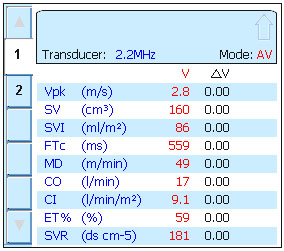
The most striking features are a CO of 17 L/min, CI of 9.1 L/min/m2, SV of 160ml and an SVR of 181! In addition, the Vpk shows that blood is being ejected at high velocity from the ventricle. Looks pretty convincing for septicaemia doesn’t it! It is hard to imagine that with a CI of 9.1 this man could have cardiac failure, but his SMII was just 0.63 W/m2 (normal 1.6 – 2.2 W/m2). His high CO and SV are possible only because his SVR is so low. His DO2 was 3,104ml/min, or over twice the normal value for a man of his size (1,300ml/min or about 15ml/kg).
So how do we treat this? Clearly he needs vasoconstriction in the form of a vasopressor to raise the SVR and thereby the BP, but does his heart have sufficient power to handle an increase in afterload? Let’s see. He was treated with an infusion of noradrenaline 100ng/kg/min which increased his BP to 97/58. The infusion rate was increased to 200ng/kg/min. His BP rose to 114/62.
Hey, looks like we’ve solved the problem, his BP is normal again. But by now you know that this is a dangerous conclusion because blood pressure does not mean blood flow. We don’t believe anything until we see the haemodynamic figures. The registrar writing “haemodynamically stable” in the notes on the basis of BP and pulse alone is not going to convince us budding haemodynamicists!
Here is his second USCOM.
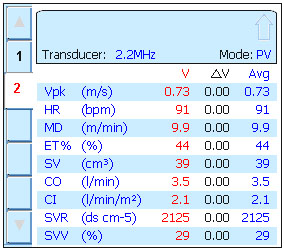
The noradrenaline certainly increased his SVR. It is now well above 1600, the upper limit of normal. His CI has fallen from 9.1 to 2.1, a figure which is clearly inadequate, given that cardiac failure is defined as a CI at rest of <2.4 L/min/m2. His DO2 has plummeted from over 3,000ml/min to just 652ml/min, almost exactly half the normal value. Reducing his noradrenaline caused his BP to fall back to 93/57. So what can we do?
Well let’s look at his inotropy index. On this second reading his SMII had increased to 1.13W/m2, better but still well below normal. We need more inotropy, but we cannot vasoconstrict him any further, in fact we need to allow him to vasodilate somewhat. The answer is to add in dobutamine. This will increase his inotropy to increase CO, and even though we allow his SVR to fall a little, as BP = CO x SVR a bigger gain in CO would outweigh a smaller fall in SVR, so we could still make a profit on the deal.
This is his fourth USCOM result. At this stage he is on noradrenaline at 200ng/kg/min and dobutamine 8mcg/kg/min. His BP is 122/66.
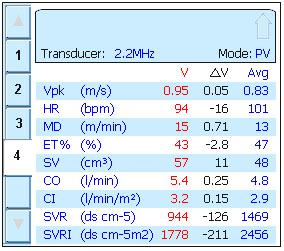
Job done! The CO and CI are normal. The SVR is normal. The BP is normal. The DO2 is 1018ml/min. This is still a little lower than we might like, but certainly adequate and 56% better than our second reading. His SMII was 1.48W/m2, not quite normal, but much better than the first or second readings. In fact we increased his dobutamine to 10mcg/kg/min, which increased SMII to 1.56, which increased his CO to 6.1 and his CI to 3.6. His SVR fell a little to 736, and his BP remained stable at 124/62. But what happened to his DO2? This increased to 1,162ml/min, not quite perfect, but near enough!
Balancing inotropes, or even using one single inotrope to its best effect, is a desperately difficult clinical skill to learn. By using the USCOM and SMII the job becomes a case of “painting by numbers”. There is still some skill and wisdom involved, but it is so much easier than clinical acumen alone, and there is absolutely no guesswork involved!
Fluid Resuscitation Alone.
But, I hear you ask, would fluids alone have been able to get the job done? It certainly wasn’t looking very promising after 4 litres of saline was it?! If we consider his initial SMII value, then he must be on the lower, flatter Frank-Starling curve. As such, increasing preload with extra fluid will give us a minimal increase in stroke volume at best, and risk overloading the ventricle with a fall in stroke volume at worst. Is there a point where inotropy is sufficient to give us a good chance of resuscitation with fluid alone? The answer is yes, and appears to be when the SMII is greater than 1.2W/m2. Below this value the response to fluid alone is disappointing and inotropes are usually needed.
By the way, did you spot that his MD changed from hyperdynamic at 49m/min to hypodynamic at 9.9m/min and then up to normodynamic at 15m/min and finally up to 17m/min after the dobutamine was increased to 10mcg/kg/min? (Normal range in adults is 14-22m/min.) This leads us to another area where SMII can be very useful, the ratio between potential energy and kinetic energy, the P:K ratio or PKR.
|

